Dear Dr Pate,
Dear Dr Pate,
I’ve read some of your (awesome) posts and have a random question I’m hoping you can answer! 🙂 I know of a mom whose son was forcibly retracted when he was 7 months old. Unfortunately, she was told that after that point, she needed to continue doing it, which she did for another year following that incident. Now she knows that was wrong. The problem is that he’s fully retractible now (even though not “naturally” so), and she doesn’t know if she should continue asking him to retract himself to clean it (as she would a naturally retractible child), or not. He’s only 2 years old, and resistant to doing so. I’m inclined to say leave it alone and that just soaking in the bath will be good enough, but wanted to double-check. If he doesn’t retract to clean, would it encourage adhesions or infection?
Dear KD,
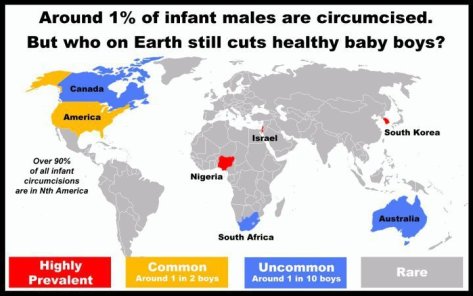
Thank you for your kind comments and your excellent question! I am inclined to tell her to leave it alone as well given that kiddos do not have the same amount of body secretions as teens and adults. Likewise, I can’t image that other cultures around the world pay even a 10th of the interest in either the excision or maintenance of the foreskin as we do in the U.S. Do little girls really need to be taught anything more to wash briefly in the tub? The same should apply to little boys. However, I am not a pediatrician so I asked my colleagues for their opinions which follow below. Best of luck to the little tyke and thanks again for writing.
Sincerely,
James Pate, MD
http://jamespatemd.com
I agree with you and would have advised the same. If he is resistant to retraction, I would leave it alone. It may re-adhere, but I would imagine that it will detach over time without undue intervention despite the earlier forcible retraction. If not, he can use steroid cream if indicated. I don’t see it becoming infected.
On the other hand he may become more amenable to retraction and cleaning in the coming months which would make it a non-issue. He may be objecting because he’s two years old. But I see no reason to compel him to do something he doesn’t want to do at this time.
―Dr Paula Brinkley, pediatrician
I just wanted to assure you that your advice was just right! We need not retract the eyelid to wash under it, and mucous membrane will keep adjacent tissues from adhering one to the other. In most non-circumcising countries, from what men have told me, they often are taught little and generally figure out hygiene on their own. If they are told something, it’s usually around puberty, probably when secondary sex hormones are produced.
We don’t teach girls to pull their prepuce back to wash under it and we don’t put Q-tips or anything else into their vaginas to wash them. The body is self-cleaning. And, little boys need a normal sense of unconcerned boyhood. The baby’s objections to having his foreskin messed with is the message to which everyone should listen.
There are three great articles that you might find helpful at http://www.nocirc.org/articles. They are:
- Unnecessary Circumcision, by George Denniston, MD. The Female Patient, July 1992.
- The Case Against Circumcision, by Paul M. Fleiss, MD, MPH, FAAP. Mothering Magazine, Fall 1997.
- Protect Your Uncircumcised Son, by Paul M. Fleiss, MD, MPH, FAAP. Mothering Magazine, November/December 2000.
―Marilyn Milos, RN, Executive Director, National Organization of Circumcision Information Resource Centers (NOCIRC)
In my opinion, you don’t have to be a pediatrician to answer this question – most pediatricians don’t know anything about taking care of the foreskin anyway! – so I’m going to offer my own take on this.
There are no controlled studies on correct care of the intact penis, so the best we have to go on is a good understanding of the structure and development of the foreskin, plus common sense.
The few studies that I know of that looked at retractability, foreskin hygiene, and outcomes are so methodologically problematic and ignorant of the natural development of the foreskin as to be completely worthless guides (Kalcev 1964, Krueger and Osborn, 1986).
Most of the “literature” on care of the intact penis are merely opinion pieces. One would hope that this “opinion” would be based on a solid knowledge of the development of the intact penis, and/or extensive experience in conservative care of the intact penis, but unfortunately this is not the case, as we all know, and there is a lot of mistaken and potentially harmful advice given.
“I did an inservice on care of the intact penis 6+ years ago where I dug up as much literature on it as I could (17 articles, 2 of which were from CIRP and NOCIRC). I am attaching a summary of some of the advice from these handouts that I posted at Mothering.com some years back, plus some additional quotes that support the idea of “leave it alone”.
Here’s the general consensus from these handouts:
- If the FS is non-retractable, no matter how old the boy is, all that need be done is to wash off the outside. PERIOD.
- Once the FS is retractable AND the boy is developmentally able (generally have the motor dexterity and ability to follow instructions by about age 4-5), he can be taught to retract, rinse, replace. [Note, this makes the idea of requesting a 2 year old to retract and clean himself seem pretty pointless.]
Sources that specifically mention frequency suggest:
- In childhood: this rinsing might be done say only “occasionally”
- By puberty: more “regular”, or “daily” rinsing is suggested
Although some older articles will recommend that parents retract the child (based, I believe on a preconception of the foreskin as problematic, and ignorance of the natural development of the intact penis), most do NOT say this, and a number do support the idea of leaving it alone (see my Mothering post attachment). In fact there is one great quote from Canadian pediatric urologist Peter Anderson stating that “there’s no evidence there’s any need to clean under the foreskin before puberty.”
Remember that the foreskin is designed to keep the ooky stuff out (tight outlet in childhood, sphincter-like action of the peripenic muscle), and that it is flushed outward multiple times a day with sterile urine, thus keeping itself clean.
As a John Geisheker likes to point out, “Our primate predecessors were unlikely to head down to a nearby river every day to scrub their children’s genitals. Nature would quickly eliminate those who needed such care. Only those tough enough to not require genital cleansing would have survived. We are those survivors. … Mid-19th century English-speaking boys and girls did not suddenly require aggressive genital hygiene when their ancestors, for hundreds of generations, survived nicely on benign neglect.”
If this 2-year-old is resistant to having his foreskin retracted, by all means, leave it alone! It is unnecessary from a hygiene point of view, and could be more psychologically distressing than its worth. He will discover the joys of retracting himself when he’s ready and interested himself. In the meantime, it is quite possible that just playing with his penis in clean tub water might be all the cleaning needed. Since the average age to full retractability is somewhere are age 10, I would encourage this young mom to sit back, respect her son’s own time table and emotional boundaries, and just let nature take its course.
―Gillian Longley RN, BSN, MSS, Colorado NOCIRC
Rather than re-invent the wheel and write a longish, potentially unwelcome, or over-obvious email, I am attaching several articles we at DOC wrote for Psychology Today magazine on this very issue.
The short answer, (which I suspect you know instinctively), is that urine is sterile and the boy-child is ‘washed’ at each urination. The notion that intact (not C’d) boys need special hygiene is an invented one of Anglophone origin, its sources easily traced to the mid 19th century, a time of great anxiety about masturbation (even among toddlers) as a source of disease. This was before Koch (1879) and others identified pathogens.
In evolutionary terms, the notion that boys need special genital hygiene makes no sense. Our primate ancestors were likely far more concerned with foraging for food and finding a safe place to sleep each night. There was no time or motive to scrub the genitalia of their offspring (and my primatologist neighbor tells me no such behavior has ever been seen in the wild).
We are their descendants who never needed any such care. The infant vulva and infant penis, like the infant eyes and mouth, are self-defending and self-cleaning. It could hardly be otherwise.
―John V. Geisheker, J.D., LL.M. Executive Director, General Counsel, Doctors Opposing Circumcision (D.O.C.)