A Public Apology to My Circumcised Son is another post I came across while catching up on my break. It was posted 11/21/10 on Peachy Keen Birth Services.
A Public Apology to My Circumcised Son is another post I came across while catching up on my break. It was posted 11/21/10 on Peachy Keen Birth Services.
“My Little Buster,” the distraught mother writes, “I’m so sorry. How else do I begin this?… As a parent, there will be a million things you will look back on and think ‘Gee… I wish I would have done that differently…’… But how in the hell do I apologize for having part of your genitals amputated for NO MEDICAL REASON? When you were less than 24 hours old!… So for all of the parenting moments I look back upon, wishing I could re-do, having you circumcised is the only one I have utter remorse for. With much, much love, Your Mommy.”
The post struck a cord in me because I too carry this burden, and I echo the sentiments of this mother.
When my son was born in 1998 — in my former life as a closeted, gay, married, mechanical engineer — my ex-wife and I had little discussion on the matter. I am circumcised, my father is circumcised and her father and brother are circumcised. Why wouldn’t we do to our son what was a norm for our family? We didn’t understand the risks. We didn’t understand the permanent damage that we were condoning. We did not understand the history of circumcision in the U.S. nor its root in puritanical aims to deter masturbation. We were simply uninformed and did not understand the gravity of our decision to circumcise our son.
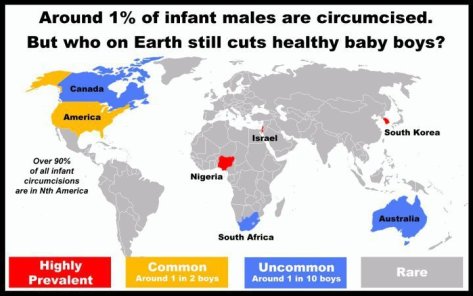
Now it is too late. We stole that choice from him and his body is permanently altered. I have apologized to him. The tears ran down my cheeks. He has forgiven me but at his young age he cannot comprehend the consequences of that decision. Do not repeat our mistakes. Leave your sons whole as nature/god intended them to be. Allow them the autonomy over their bodies that is rightfully theirs alone. Let’s end this barbaric custom of infant genital mutilation!
– James Pate, MD



 Via the Washington Post, the Associated Press reports that World War II Navy veteran, Melvin Dwork, has finally won his decades long fight: changing his “undesirable” discharge for being gay to “honorable”. The change is more than saving face, “he will now be eligible for the benefits he had long been denied, including medical care and a military burial.” This decision is hopefully only the first of many given that over 100,000 soldiers have been discharged since WWII and robbed of their honor and military benefits simply for being gay. “Don’t Ask Don’t Tell” officially dies tomorrow, 9/20/11.
Via the Washington Post, the Associated Press reports that World War II Navy veteran, Melvin Dwork, has finally won his decades long fight: changing his “undesirable” discharge for being gay to “honorable”. The change is more than saving face, “he will now be eligible for the benefits he had long been denied, including medical care and a military burial.” This decision is hopefully only the first of many given that over 100,000 soldiers have been discharged since WWII and robbed of their honor and military benefits simply for being gay. “Don’t Ask Don’t Tell” officially dies tomorrow, 9/20/11.